Dense Breast Legislation in the United States – how does it work?

In March 2019, the U.S. Food and Drug Administration (FDA) introduced new guidelines for mammography screening facilities. According to them, women with so-called dense breasts should be provided with better information about the structure of their breasts and the effectiveness of the test itself in such cases. So how has the law changed in the United States and what we now call the ‘Dense Breast Legislation’?
There are a number of legal changes that are now in effect for facilities offering mammography screening in the US. As a reminder, mammography is one of the most popular methods used for early screening of breast cancer.
The law first went into effect in the state of Connecticut in 2009, and soon other states followed, by making changes in local legislatures. This law obliges mammography facilities to inform patients in case dense breasts were identified on a mammogram. The intended outcome is increased public awareness of dense breasts and risks associated with them.
What are dense breasts?
Dense breasts are common among women. They are built of glandular and connective tissue rather than fatty tissue. It is estimated that about half of all women in the world have dense breasts. Unfortunately, mammography is less useful for breast cancer screening purposes in dense breasts. In addition, women with dense breasts are more likely to develop breast cancer. Learn more about dense breasts and what they are.
Rights of women with dense breasts
In March 2019, the FDA introduced nationwide standards on patients’ right of information about breast structure, specifically about dense breasts. From that point forward, facilities performing mammograms are required to:
- develop a clear system of patient information materials (including flyers) about different breast structures,
- develop a system for describing the results of the test so that every patient knows the diagnostic value of the test for her breast structure,
- inform the referring doctor that the patient has dense breasts
- inform patients with dense breasts of the lower diagnostic value of the test and the increased risk of disease
- inform patients with dense breasts of the right to consult their case with the attending physician, who can answer all their questions and determine the further course of action,
- determine the qualifications of the doctor interpreting mammogram results in that facility.
These developments were intended to build awareness of the problem of dense breasts and to draw attention to the limited diagnostic options in this area. Since then, screening facilities operate according to established standards and women in the U.S. who undergo mammography screening are better informed.
Information for patients with dense breasts – current status
As of now [as of January 5, 2021], 37 U.S. states and the District of Columbia have to a greater or lesser extent enacted appropriate regulations involving so-called ‘dense breast legislation’. In some states, patients only need to be told what dense breasts are and the risks associated with them, and some states also require that each patient be informed after the mammogram whether or not this breast structure was found.
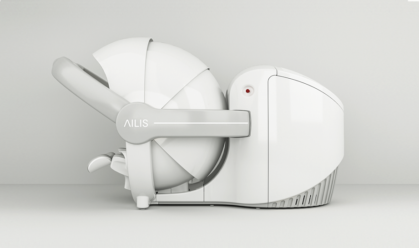
Check how does AILIS Breast Cancer Prediction Technology works for woman with dense breasts
References:
- Dehkordy, Soudabeh Fazeli, and Ruth C. Carlos. “Dense Breast Legislation in the United States: State of the States.” Journal of the American College of Radiology, vol. 10, no. 12, Dec. 2013, pp. 899–902, 10.1016/j.jacr.2013.09.007. Accessed 9 Jan. 2021.
- “National Reporting Standard.” DenseBreast-Info, Inc., 28 Mar. 2019, densebreast-info.org/legislative-information/national-reporting-standard/. Accessed 9 Jan. 2021.
- “Patient Questions And Answers.” DenseBreast-Info, Inc., 23 Nov. 2020, densebreast-info.org/for-patients/patient-questions-and-answers/. Accessed 9 Jan. 2021
- “State Legislation Map.” DenseBreast-Info, Inc., 5 Jan. 2021, densebreast-info.org/legislative-information/state-legislation-map/. Accessed 9 Jan. 2021.